My First Fifty Years
by John R Bennett
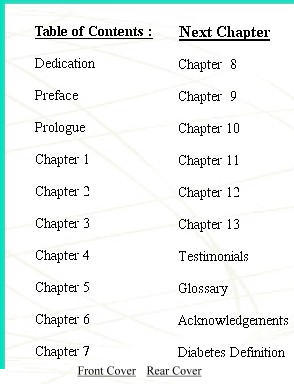
Glossary
Unless otherwise noted, words and terms from MEDLINEplus
http://www.nlm.nih.gov/medlineplus/dictionaries.html a web version of "U.S. National Library of Medicine (NLM), 8600 Rockville Pike, Bethesda, MD 20894".
Other sources:
A1C - see Hb A1C
blood-glucose level
|
Most dietary carbohydrate eventually ends up as glucose in the blood. Excess glucose is converted to glycogen for storage by the liver and skeletal muscles after meals. Glycogen is gradually broken down to glucose and released into the blood by the liver between meals. Excess glucose is converted to triglyceride for energy storage. Glucose is a major source of energy for most cells of the body. Some cells (for example, brain and red blood cells), are almost totally dependent on blood glucose as a source of energy. The brain, in fact, requires that glucose concentrations in the blood remain within a certain range in order to function normally. Concentrations less than about 30 milligrams per deciliter (mg/dl) or greater than about 300 mg/dl can produce confusion or unconsciousness. |
blood-glucose monitor
| Blood sugar testing, also called "self-monitoring," is done using a special meter called a glucometer to check the amount of glucose in a drop of blood. Testing is usually done before meals and at bedtime, though more frequent testing may be needed during times of illness or stress. If it is done on a regular basis, testing informs the diabetic patient and their healthcare provider how well diet, exercise, and medication are working together to control their diabetes. |
carbohydrate
|
The primary function of carbohydrates is to provide energy for the body, especially the brain and the nervous system. The body breaks down starches and sugars into a substance called glucose, which is used for energy by the body. It is recommended that somewhere between 40 to 60% of our total calories come from carbohydrates, preferably from complex carbohydrates (starches) and naturally occurring sugars rather than processed or refined sugars. High-sugar foods are simple carbohydrates that provide calories, but minimal nutritional benefits. On the other hand, complex carbohydrates provide calories, vitamins and minerals as well as fiber. Therefore, it is wise to limit processed and refined sugars. |
clinitest
|
A screening test to detect the presence of various substances in the urine that chemically react with an indicator metallic dye (cupric sulfate). The most common reducing substances examined include glucose or galactose. If the Clinitest tablet turns blue, this indicates the present of a urinary reducing substance such as glucose (as seen in diabetes). A simple urine dipstick test that is specific for glucose can be performed. If the dipstick test is positive, then you have a high level of glucose in the blood, and the glucose is spilling over into the urine. |
conventional control
|
Diabetes results from deficient insulin or insensitivity to insulin. Type I diabetics require daily injections of insulin. Injection of too much or too little insulin can be dangerous. Normal values : 64 to 126 mg/dl Note: mg/dl = milligrams per deciliter. |
dawn phenomenon [MEDLINEplus - On-line Medical Dictionary (CancerWEB)]
| Abrupt increases in fasting levels of plasma glucose concentrations between 5 and 9 a.m., in the absence of antecedent hypoglycaemia; occurs in diabetic patients receiving insulin therapy. |
DCCT
| The Diabetes Control and Complications Trial (DCCT) studied the effects of tight blood sugar control on complications in Type 1 diabetes. Patients treated for tight blood glucose control had an average HbA1c of approximately 7 percent, while patients treated less aggressively had an average HbA1c of about 9 percent. At the end of the study, the tight blood glucose group had dramatically less kidney disease, eye disease, and nervous system disease than the less aggressively treated patients. |
diabetes (diabetes mellitus) - please refer to chapter "Diabetes Definition"
| Diabetes is a life-long disease of high blood sugar caused by too little insulin, resistance to insulin, or both. |
diabetic [Merriam-Webster's Collegiate® Dictionary]
| n. : a person affected with diabetes |
diabetic coma
| A state of unawareness or loss of consciousness with a lack of ability to respond. Can be caused by either hypoglycemia or hyperglycemia. |
exchange [JRB]
|
A serving of food that contains known and relatively constant amounts of carbohydrate, fat, and/or protein. The food used in an exchange is usually weighed or measured. The exchanges are divided into several groups: milk, fruit, meat, fat, bread, and vegetables. For complete exchange lists refer to the American Diabetes Association website searching for Exchange Lists. |
fasting blood glucose
|
FBS; Blood sugar levels; Fasting blood sugar This test is used to evaluate glucose (blood sugar) levels. It may be used to diagnose diabetes, monitor diabetic control, or as a screening test. Nothing By Mouth (NBM) eight hours prior to early morning testing. |
fluorescein scan [Merriam-Webster's Collegiate® Dictionary]
| Fluorscein is a yellow or red crystalline dye with a bright yellow-green fluroescence in alkaline solution - injected into a vein fluorescein is used to highlight and take photos of proliferated blood vessels in the retina. |
gestational diabetes - see also chapter "Diabetes Definition"
| ... high blood glucose at any time during pregnancy |
glucagon
|
Glucagon levels may be measured in persons with chronically or repeatedly low blood sugar (glucose) levels. Glucagon is a peptide (protein) hormone that is released from the pancreas. The main function of glucagon is to stimulate the liver to release glucose between meals (glucose is normally stored in the liver as glycogen), and release of amino acid (alanine) from muscles. Glucagon also increases fatty acid release from adipose (fat) tissue and synthesis of glucose (from lactate or amino acids) in the liver. As the level of glucose is decreased, glucagon secretion from the pancreas increases, and vice versa. |
glucolysis [Merriam-Webster's Collegiate® Dictionary]
| the enzymatic breakdown of a carbohydrate (as glucose or glycogen) by way of phosphate derivations |
glucose
| Glucose is a major source of energy for most cells of the body. Some cells (for example, brain and red blood cells), are almost totally dependent on blood glucose as a source of energy. The brain, in fact, requires that glucose concentrations in the blood remain within a certain range in order to function normally. |
glucose tolerance - see glucose-tolerance test
glucose-tolerance test
|
Glucose is the sugar that the body uses for energy. Patients with diabetes mellitus have high blood glucose levels. Glucose tolerance tests are one of the tools for making the diagnosis of diabetes. The most common glucose tolerance test is the oral glucose tolerance test (OGTT). After an overnight fast, a patient drinks a solution containing a known amount of glucose. Blood and urine are obtained before the patient drinks the glucose solution, and blood is drawn again every hour after the glucose is consumed for up to three hours. |
glycogen
| Glycogen is glucose in storage form in the liver. It may be broken down to form blood glucose during an insulin reaction or during a fast. |
glycohemoglobin - see Hb A1C
glycosolated hemoglobin - see Hb A1C
gram [JRB]
| 1 pound [16 ounces] equals 453 grams |
Hb A1C
|
Hb A1c; Hemoglobin - glycosylated; GHb; Glycohemoglobin; Diabetic control index
This test is used to measure blood sugar control in individuals with diabetes mellitus.
In normal individuals a small percentage of the hemoglobin (Hb) molecules in red blood cells become glycosylated (that is, chemically linked to glucose). Glycosylated hemoglobin can be separated from normal HbA by electrophoresis (a laboratory technique) into 3 fractions called HbA1a, HbA1b, and HbA1c. Normally only HbA1c is quantitated. The percent of glycosylation is proportional to time and to concentration of glucose. In other words, older red blood cells will have a greater percent of GHb and poorly-controlled diabetics (with periods of time where they have high concentrations of blood glucose) will have a greater percent of GHb. |
health-care team [JRB]
| The group of professionals who help manage diabetes and which may include a physician, registered dietitian, and certified diabetes educator, ophthalmologist, podiatrist, endocrinologist or other specialists. |
hyperglycemia [MEDLINEplus - MedicineNet.com Medical Dictionary (MedicineNet, Inc.)]
|
A high blood sugar. An elevated level specifically of the sugar glucose in the blood.
The term "hyperglycemia" comes from the Greek "hyper-" = high, over, beyond, above + "glykys" = sweet + "haima" = blood. High sweetness (sugar) in the blood. |
hypoglycemia
|
Insulin shock; Insulin reaction; Low blood sugar Hypoglycemia occurs when your body's blood sugar, or glucose, is abnormally low. The term insulin shock is used to describe severe hypoglycemia that results in unconsciousness. |
IMHO [JRB] In My Humble Opinion
insulin
| Insulin is a hormone released from the beta cells of the pancreas. Insulinís most important function is to facilitate glucose uptake by a variety of tissues, especially adipose (fat) and skeletal muscle. Insulin also stimulates the synthesis and storage of triglycerides and proteins. Insulin is the most important regulator of blood glucose. High blood glucose (such as exists shortly after a meal) stimulates the release of insulin, whereas low blood glucose levels inhibit insulin release. |
insulin-dependent diabetes mellitus (IDDM) - see Type-I Diabetes
insulin reaction - see hypoglycemia
islets of Langerhans - see pancreas
isophane insulin
| NPH (neutral protamine Hagedorn) insulin, a neutral pH, intermediate-acting insulin. |
Joslin, Elliott P (Proctor), 1869-1962 [Michael Bliss's The Discovery of Insulin]
|
Elliott Joslin ['the master clinician of diabetes' who
worked at the time of insulin's appearance] devoted his
life to the treatment of diabetes. He also realized
that the disease was far from solved by insulin.
He considered insulin the end of one era in diabetes
management, not the end of diabetes. "It has been forced upon me that diabetic gangrene is not heaven sent but earth born." E.P.Joslin 1934 (61) |
juvenile diabetes - see Type-I Diabetes
| Now called Type-I or insulin-dependent diabetes mellitus (IDDM). |
ketones
| Ketones (beta-hydroxybutyric acid, acetoacetic acid, and acetone) are the end-product of rapid or excessive fatty acid breakdown. As with glucose, ketones "spill over" into the urine when the blood levels are above a certain threshold. Fatty acid release from adipose tissue is stimulated by a number of hormones including glucagon, epinephrine, and growth hormone. The levels of these hormones are increased in starvation, uncontrolled diabetes mellitus, and a number of other conditions. |
metabolism
| Physical and chemical processes within the body related to body functions. Processes of energy generation and use; including nutrition, digestion, absorption, elimination, respiration, circulation, and temperature regulation. |
mg/dl (milligrams per deciliter) [JRB]
| The unit of measure used to describe blood-glucose levels. |
ophthalmology [Merriam-Webster's Collegiate® Dictionary]
| a branch of medical science dealing with the structures, functions, and diseases of the eyes (see also retinopathy) |
optometry [Merriam-Webster's Collegiate® Dictionary]
| the art or profession of examining the eye for defects and faults of refraction and prescribing correctional lenses or exercises but not drugs or surgery |
pancreas
| An organ called the pancreas makes insulin. The role of insulin is to move glucose from the bloodstream into muscle, fat, and liver cells, where it can be used as fuel. People with diabetes have high blood glucose. This is because their pancreas (islets of Langerhans) does not make enough insulin, or their muscle, fat and liver do not respond to insulin normally, or both. |
photocoagulation [Merriam-Webster's Collegiate® Dictionary]
| a surgical process of coagulating tissue by means of a precisely oriented high-energy light source (as a light beam) |
regular insulin
| Regular or short-acting insulin (human) usually reaches the bloodstream within 30 minutes after injection. It peaks anywhere from 2 to 3 hours after injection, and is effective for approximately 3 to 6 hours. |
retina
| Internal layer of the eye that receives and transmits focused images. The retina is normally red due to its rich blood supply. It can be seen with an ophthalmoscope, which allows the examiner to see through the pupil and lens to the retina. Changes in color of the retina or changes in the appearance of retinal blood vessels may indicate disease. Changes in color perception and in vision also indicate disease and indicate the need for a retinal examination. |
retinopathy (see also photocoagulation)
| Disease of the retina. Retinopathy occurs in persons with prolonged, poorly controlled diabetes and involves abnormal growth of and bleeding from the capillary blood vessels in the eye. |
self-monitoring of blood glucose (SMBG)
| A technique of testing a person's blood-glucose level in order to determine the body response to activity, food, and medication. |
subcutaneous
| Beneath or under the skin. Cutaneous means of or in the skin. |
sugar - see also carbohydrates
| Glucose is the sugar that the body uses for energy. |
Type-I diabetes - see also chapter "Diabetes Definition"
|
[Insulin Dependent Diabetes Mellitus (IDDM)] ...usually diagnosed in childhood. The body makes little or no insulin, and daily injections of insulin are required to live. Without proper daily management, medical emergencies can arise. |
Type-II diabetes - see also chapter "Diabetes Definition"
|
[Non-Insulin Dependent Diabetes Mellitus (NIDDM)] ... ...far more common ( [than Type-I Diabetes] - about 90% of all diabetes cases) and usually occurs in adulthood. The pancreas does not make enough insulin to keep blood glucose levels normal, often because the body does not respond well to the insulin. Many people with Type 2 diabetes do not even know they have it, although it is a serious condition. Type 2 diabetes is becoming more common due to the growing number of older Americans, increasing obesity, and a lack of exercise. Without proper management, long-term health risks such as heart disease, stroke, and kidney failure can occur. |